Deep Vein Thrombosis (DVT)
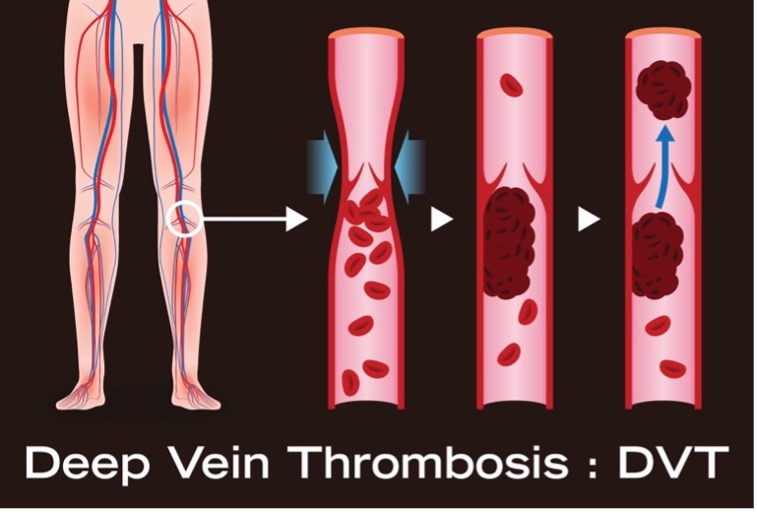
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs. Deep vein thrombosis can cause leg pain or swelling. Sometimes there are no noticeable symptoms.
Deep vein thrombosis can be serious because blood clots in the veins can break loose. The clots can then travel through the bloodstream and get stuck in the lungs, blocking blood flow (pulmonary embolism).
Symptoms
In some cases, there may be no symptoms of DVT. If symptoms do occur, they can include:
- pain, swelling, and tenderness in one of your legs (usually your calf or thigh);
- a heavy ache in the affected area;
- warm skin in the area of the clot; or
- red skin, particularly at the back of your leg below the knee.
DVT usually (although not always) affects one leg. The pain may be worse when you bend your foot upward towards your knee.
Risk Factors
Anyone can develop DVT, but it becomes more common over the age of 40. Besides age, there are also some other risk factors, including:
- having a history of DVT or pulmonary embolism;
- having a family history of blood clots;
- being inactive for long periods, such as after an operation or during a long journey;
- blood vessel damage, where a damaged blood vessel wall can result in the formation of a blood clot;
- having certain conditions or treatments that cause your blood to clot more easily than normal, such as cancer, heart and lung disease, thrombophilia, and Hughes syndrome;
- being pregnant, as your blood also clots more easily during pregnancy; and/ or
- being overweight or obese.
The combined contraceptive pill and hormone replacement therapy (HRT) both contain the female hormone estrogen, which causes the blood to clot more easily. If you’re taking either of these, your risk of developing DVT is slightly increased.
Diagnosis
When you suspect a blood clot or are referred, our vascular team will begin by asking you about your symptoms and medical history. A duplex venous ultrasound scan may be done in the office to confirm DVT and can be used to detect clots in your veins or insufficient blood flow.
Treatment
Treatment for DVT usually involves taking anticoagulant and thrombolytic medications. These reduce the blood’s ability to clot and prevent existing clots from getting bigger.
If a very large blood clot has formed and threatens to break loose into the bloodstream, a minimally invasive surgical procedure may be recommended to remove the clot. These procedures may also be performed for people who cannot take anticoagulants, or blood thinners, and thrombolytics, also known as clot-busting medicines, because of a health condition such as a bleeding disorder.
Thrombectomy
A surgical thrombectomy is considered a minimally invasive surgery and can be done in our office on an outpatient basis.
In a thrombectomy, a contrast dye is injected which helps locate the clot using X-ray guidance. The clot can usually then be removed using a thin tube called a catheter, which is a long, flexible, hollow tube that is inserted through a vein in the groin or arm and threaded to the location of the blood clot.
Patients remain awake for the procedure and receive a mild sedative beforehand. If you have multiple blood clots, or if imaging doesn’t clearly reveal the location of the clot, doctors may use general anesthesia.
Afterward, your recovery time depends on the size and seriousness of the clot, your health, and your medical history. Your doctor may prescribe anticoagulant medications to thin the blood to prevent additional clots from forming.
What to Know about May-Thurner Syndrome
Another dangerous issue is compression of the iliac vein against the lumbar spine by an overlying iliac artery, resulting in venous insufficiency, stenosis, and obstruction. This is known as May-Thurner syndrome.
May-Thurner syndrome makes it harder for blood to flow back to your heart. Instead, it may pool in your legs and can develop into a DVT.
The standard treatments for May-Thurner syndrome (MTS) include venoplasty, which uses a balloon catheter to open blocked veins, and iliac vein stenting, where a stent is inserted to keep the blood flow channel open. In more severe cases, bypass surgery, angioplasty, or repositioning of the right iliac artery may be necessary.
If you have leg swelling, leg pain, cramping, or change in skin color on the leg, talk to your primary care provider. Or, contact our office to schedule a consultation with our Vascular Center. Call (860) 522-0604.

Our Vascular Center Team