Testing
Testing is a critical aspect of cardiovascular care and allows us to diagnose issues and assess the severity so we can determine the appropriate treatment plan. Our testing labs are accredited by the Intersocietal Accreditation Commission which means we meet the highest standards of patient care and safety. Click on the test below to learn more about what each test entails.
To learn more about the wide range of tests we offer, please click below.
Exercise Stress Test (without imaging)

An exercise stress test is done under the supervision of the cardiologist. For this test, you will be asked to walk on a treadmill while your heart is being monitored by a continuous ECG recording. A specially trained cardiac technologist will perform the test.
Exercise stress tests are not uncomfortable. The length and difficulty of the test is tailored to each individual patient. The entire test usually takes less than thirty minutes and most people walk on the treadmill for 6 to 12 minutes. The results of the test are available immediately and will be communicated to you and your primary care physician promptly.
Exercise stress tests are commonly used to detect the presence of coronary artery disease, abnormal heart rhythms, abnormal blood pressure response to exercise, and to evaluate exercise tolerance and exercise-related symptoms.
Instructions:
- Please do not eat or drink for four (4) hours prior to your test.
- Do not smoke for four (4) hours prior to your test.
- Wear comfortable shoes and clothing for your test.
- Take your medications as usual on the day of the test, unless your doctor instructs you otherwise.
- Please bring a list of your medications and your insurance card on the day of your test.
Stress Echocardiogram
For this type of stress test, a specially trained technologist will record several ultrasound or “echo” images of your heart at rest; this will be followed by treadmill exercise (usually for 6 to 12 minutes at a pace appropriate to the individual), and then several more ultrasound images of your heart will be taken immediately after the exercise. The stress test is performed under the supervision of a cardiologist with continuous ECG and blood pressure monitoring. The data is analyzed by the cardiologist to detect the presence of coronary artery disease (coronary artery blockages). Overall heart function and the presence of a previous heart attack (myocardial infarction) are also evaluated on this test.
This test takes approximately 45 minutes to complete.
Instructions:
- Please do not eat or drink for four (4) hours prior to the test.
- Do not smoke for four (4) hours prior to the test.
- Wear comfortable shoes and clothing for your test.
- Take your medications as usual on the day of your test, unless instructed otherwise.
- Please bring a list of your medications, your insurance card, and your co-pay (if any) to your appointment.
Dr. Granquist provides useful information on Stress Echocardiography. Click below to watch his video.
Stress Test with Nuclear Imaging

A nuclear stress test is a non-invasive test that provides your cardiologist with additional information about your coronary blood flow. The test consists of two parts, a stress component and a resting component. The test can show the size of the heart’s chambers, how well the heart is pumping blood, and whether the heart has any damaged muscle. Nuclear stress tests can also give doctors information about your arteries and whether they might be narrowed or blocked because of coronary artery disease.
Part I: Rest
- An IV is placed in your arm;
- A low level radioactive tracer is injected through the IV. There are no side effects from the injection;
- You will wait in the waiting room for your resting pictures;
- You will lie under an open camera to take images of your heart.
Part II: Stress
If you are walking on the treadmill:
- You will be connected to a heart monitor and walk on the treadmill to elevate your heart rate.
- The amount of time spent on the treadmill varies based on age and overall fitness;
- While you are walking on the treadmill, an isotope will be injected through the IV for stress pictures;
- When stress portion is over, the IV will be removed and you will wait in the waiting room for your last set of pictures;
- We recommend you eat and drink something while you wait.
If you are NOT walking on the treadmill:
- You will receive a medication called Lexiscan that dilates the arteries around the heart;
- During the test, your blood pressure and heart rhythm will be monitored;
- When the test is over, you will wait in the waiting room for your last set of pictures;
- We recommend you eat and drink something while you wait.

Results:
A nuclear cardiologist will interpret your results. If a follow-up visit is scheduled within the next few weeks, results will be discussed at that appointment. Otherwise, you can expect to receive a call from our office with your results.
Where is this test performed:
This test is available in our Glastonbury, Wallingford and Avon locations. Your test may take place all in one day or two consecutive days. This will be determined when your appointment is set up. A one-day test takes approximately three hours to complete. A two-day test takes approximately 1½ hours each day to complete.
Preparation:
Preparations for this test are very important. Please follow the instructions EXACTLY.
- No caffeine of any kind for 12 hours prior to the test, including regular and decaf coffee, regular or decaf tea, soda or chocolate
- Do not eat 4 hours before the test
- Do not smoke or vape for four hours prior to the test
- Drink plenty of water before the test, unless you have fluid restrictions
- Please bring a list of your medications, your insurance card, and your co-pay (if any) to your appointment
- We provide water and crackers for you after the stress portion of the test
- Click here for more information about medication and dietary considerations for this test
If you are or think you may be pregnant, please inform the technologist.
Clothing:
- Dress in layers as it may be cool in the office;
- If you are walking on the treadmill, wear comfortable clothes and sneakers;
- Do not use any lotion on your chest and/or arms.
Medications:
- Medications such as beta blockers, calcium channel blockers, diltiazem, metformin and insulin may be held prior to the procedure. Please refer to your cardiologist’s recommendation.
Important note:
If you must cancel your test, we require 24-hour notice. A fee will be billed for any missed appointments without 24-hour notice. The nuclear isotopes are ordered ahead of time, specifically for you. They are not returnable.
Echocardiogram
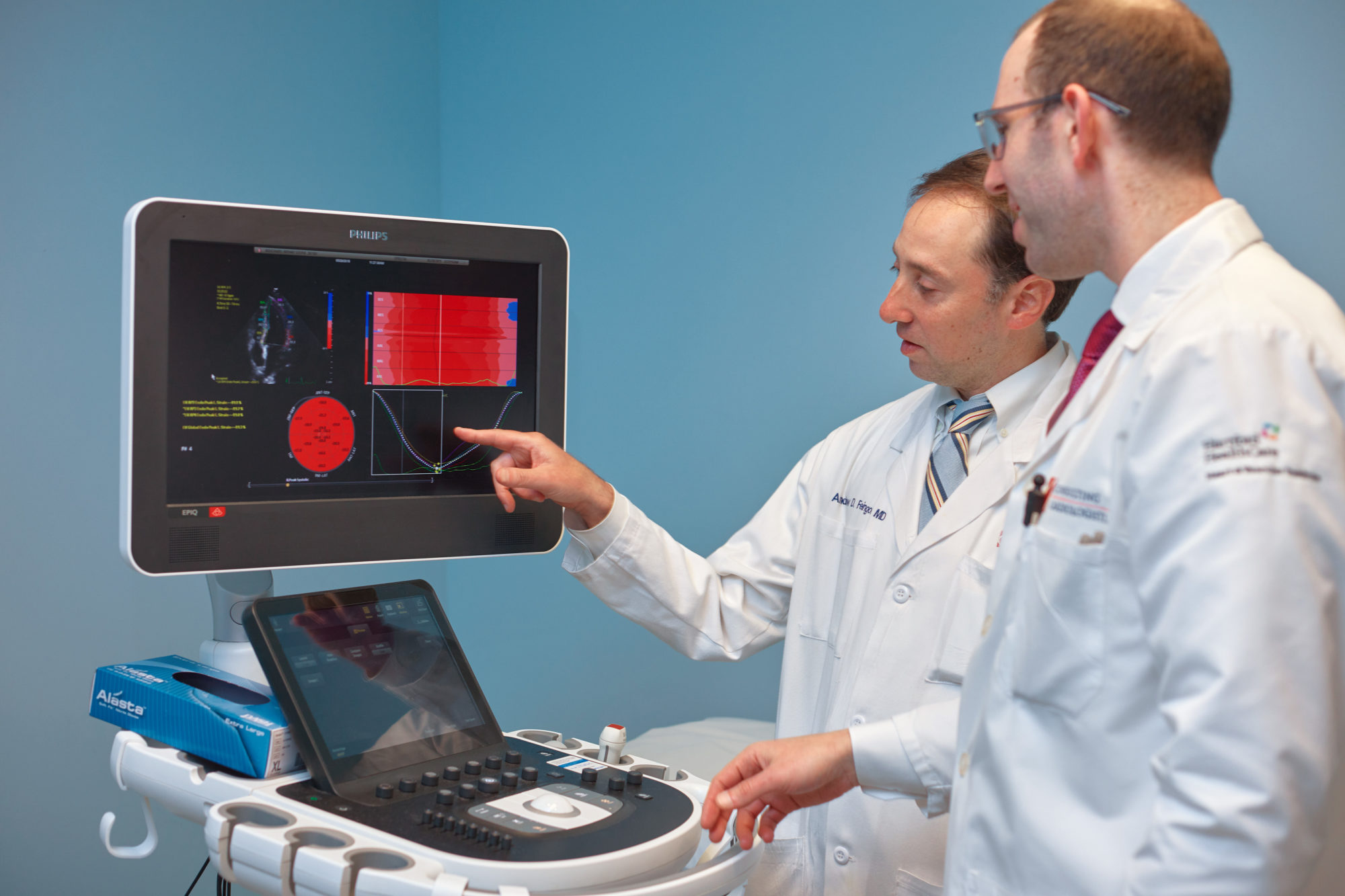
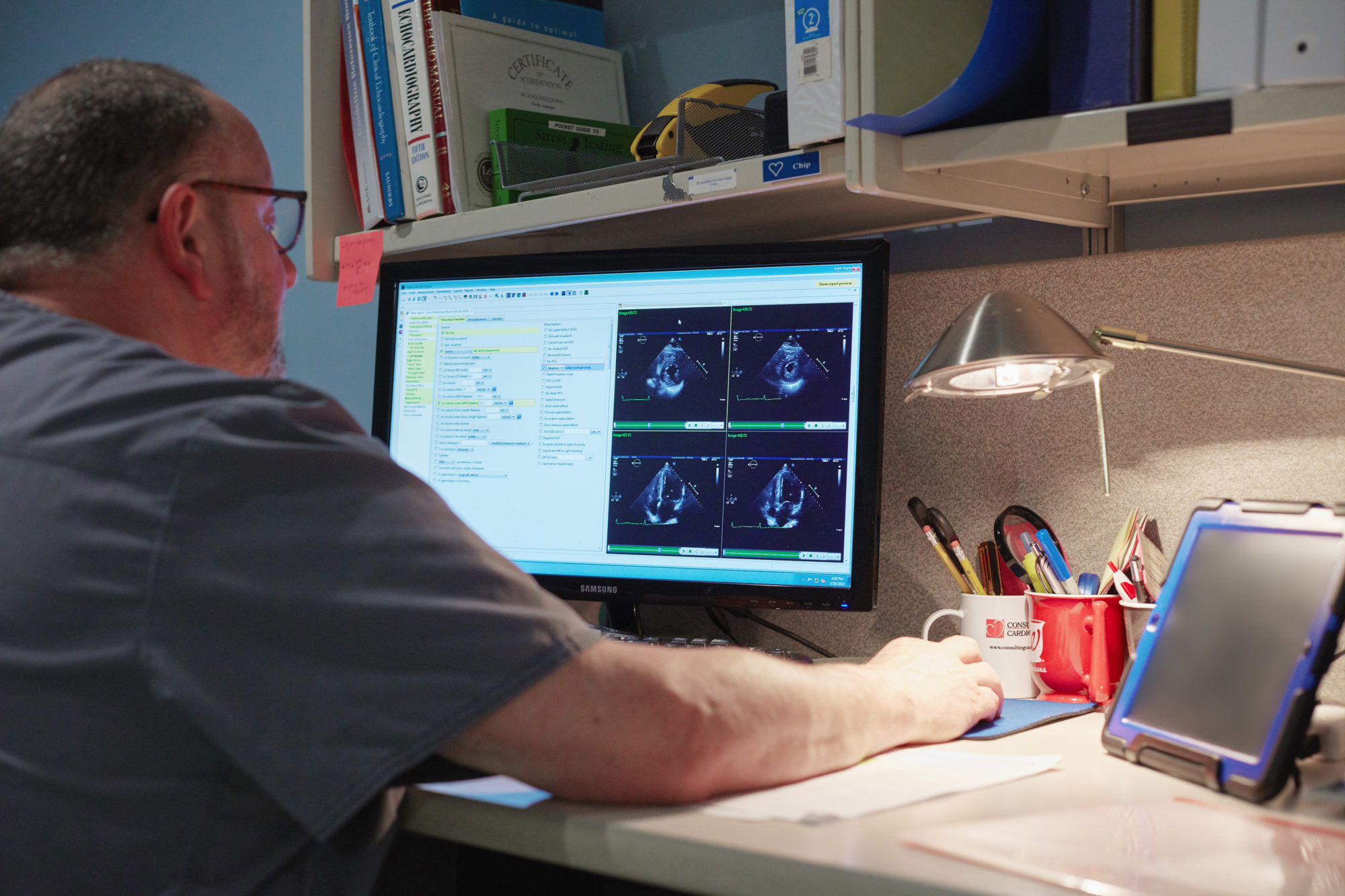
An echocardiogram, or cardiac ultrasound, is a common test used to evaluate heart function. The cardiologist can evaluate heart size and the strength of the heart “pump,” and can make sure the heart valves are functioning properly. A wide variety of heart abnormalities can be detected using this test, and echocardiograms are used to follow progress after the treatment of a heart condition as well. This information can be obtained quickly and painlessly, and it is very helpful to your doctors in determining the condition of your heart.
The test is performed by a registered cardiac technologist and is interpreted by a specially trained cardiologist. No special preparation is required on your part.
You will recline comfortably on a bed, usually on your left side, while images are obtained using a probe that is applied to the chest wall. The test usually takes about 30 minutes to perform. The post-test processing and interpretation of your test will be done after you leave, and a report will be available after your physician has reviewed the results.
This test includes real-time 2D (2 dimensional) images of the heart structures, as well as Doppler images of the heart valves to check for blood flow abnormalities; in some cases the newer 3D (3 dimensional) technology is utilized.
This test is performed in multiple offices in our accredited laboratories.
Dr. Feingold provides useful information on echocardiograms. Click below to watch his video.
Carotid Duplex Ultrasound
A Carotid Ultrasound is a simple ultrasound scan used to detect and follow the progression of cerebrovascular disease (“CVD,” or plaque build-up in the carotid arteries). The carotid arteries carry oxygenated blood from the aorta, along both sides of the neck, and are the main supply of blood to the face and brain. Detecting and treating significant plaque build-up is an important stroke prevention measure.
During the scan you will recline comfortably on an exam table, your neck will be draped, and your arteries will be imaged by a specially trained technologist using a small ultrasound probe. The test is not uncomfortable and the scan itself takes approximately 10 to 15 minutes on each side of your neck. The test is interpreted by a cardiovascular specialist.
Some common indications for this test include:
- Dizziness
- Confusion, fainting, or non-responsiveness
- Disturbances of vision or speech
- Numbness, weakness or paralysis, facial drooping
- History of previous stroke (CVA) or transient ischemic attack (TIA)
- Arterial disease in other parts of the body, such as coronary artery disease (CAD) or peripheral arterial disease (PAD)
- A “bruit,” or slightly louder blood flow sound over the carotid artery when the doctor listens with a stethoscope
There is no special preparation for the test.
Dr. Dougherty provides useful information on carotid ultrasounds. Click below to watch his video.
Peripheral Arterial Disease and Ankle Brachial Index Test (ABI)
Peripheral arterial disease (PAD) occurs when there is a build-up of cholesterol and plaque in the arteries of the lower extremities, causing decreased blood flow to the legs and feet. Signs and symptoms of peripheral arterial disease may include pain in the legs while walking that is relieved by rest, pain at rest, slow healing leg wounds, color changes in the skin, leg cramping, or reduced pulse. The groups most at risk for PAD include men and women over the age of 70. Those over the age of 50 who have a history of high blood pressure, high cholesterol, diabetes, or smoking are also at an increased risk.
The first test for PAD is often a non-invasive screening method called an Ankle Brachial Index, or an ABI. This test detects blockages in the legs by measuring segmental blood pressure measurements in the arms and the legs and comparing them.
During this test, you will recline comfortably on an exam table. A specially trained technologist will place blood pressure cuffs on both arms, and at several sites on both legs. The cuffs will be inflated one by one, and pressures and waveforms will be obtained using a special machine. The test will be interpreted by a cardiovascular specialist to determine if blood flow to the legs is less than normal. If a blockage is detected, the specialist will try to determine which artery is involved, and if the degree of PAD is serious.
After these resting measurements are obtained, you may be asked to walk briefly on a treadmill. Some of the measurements will be repeated immediately after the exercise to determine if there is a pressure drop post-exercise. This part of the test is eliminated if you cannot walk well on a treadmill.
Overall, the test is very comfortable for patients, and gives your doctor valuable information to aid in your healthcare. The test will be interpreted by a cardiovascular specialist to determine if blood flow to the legs is less than normal. If a blockage is detected, the specialist will try to determine which artery is involved, and if the degree of PAD is serious.
There is no special preparation for this test. Wear or bring a pair of lightweight shorts; patients are more comfortable during this test wearing shorts rather than a standard patient gown. Do not use any tobacco products for 30 minutes prior to arriving at the office for the test.
Holter & Event Monitors
We offer several small, portable heart monitors that can be worn easily during normal daily activities. These monitors are designed to show the cardiologist your heart activity outside the office for an extended length of time. The main reason for their use is to detect abnormal heart rhythms (arrhythmias), or to see if symptoms you may be having are associated with abnormal heart activity.
The monitor that is used to record heart activity for 24 or 48 hours is the Holter Monitor. Up to five small electrodes or “leads” are placed on the chest under your shirt; these are connected by wires to a small recorder (monitor). The recorder itself is small (like a cell phone) and can tuck into a pocket. A wireless patch monitor is also available. Heart activity is automatically recorded onto a computer chip during normal daily activity. The monitor is then returned to our office and the information is interpreted by a cardiologist.
An Event Monitor is used for a longer period of time, commonly for 30 days; although it can be worn continuously during that period, it is also possible for the patient to apply the monitor just while experiencing symptoms. This monitor is also small like a cell phone, can tuck into a pocket, and is attached to the chest wall using leads. Whenever the patient feels symptoms, a transmission is made to our office by placing the monitor over a phone. That transmission of heart activity is interpreted by a cardiologist each time. The monitor is returned after the specified length of time.
Some common reasons for monitoring include:
- Feelings of palpitations or irregular heartbeats
- Unexplained dizziness or fainting
- To determine the frequency of a known arrhythmia (abnormal rhythm)
There is no special preparation for this test, and these monitors are comfortable to wear and easy to use.
Dr. Golub provides useful information on different monitoring options. Click below to watch his video.
Ambulatory Blood Pressure Monitoring (ABPM)
We offer a small, portable blood pressure monitor that can be worn easily during normal daily activities to automatically record your blood pressure over an extended period of time (usually 24 hours) outside your doctor’s office.
Some common reasons for monitoring include:
- To identify “white coat hypertension” (high blood pressure that occurs when you are at a healthcare facility that does not occur with normal daily activities).
- To ensure your blood pressure medications are giving you adequate protection during all of your daily activities.
- To get accurate blood pressure readings while you are sleeping; sleeping blood pressure trends can aid in the diagnosis and treatment of high blood pressure.
This device can be fully concealed under a shirt or blouse. The blood pressure cuff is placed on the upper arm and is attached to the recorder by a thin blood pressure tube.
You will usually be asked to wear the monitor for 24 hours and then return it to our office for interpretation of the data. You will be able to do all of your normal daily activities, including work. It is simple to remove the monitor when taking a shower or swimming, and to reapply it when you are done. The monitor is set to auto-inflate and measure your blood pressure every 30 minutes during the day, and every hour during sleep; the information is automatically saved onto a computer chip. The monitor is comfortable and easy to use.
There is no special preparation for this test.
Electrocardiogram
An electrocardiogram, also known as “EKG” or “ECG,” is a simple, non-invasive test used to measure the electrical activity of the heart. An ECG is often included as part of your cardiac exam. ECGs are also used to follow the progression of someone undergoing treatment for a heart condition.
You will recline comfortably on an exam table; electrodes (stickers) will be placed on your chest, shoulders, and ankles. The test itself is very brief (usually less than 2 minutes), although it takes a couple of additional minutes to set up the ECG machine before the test. The test is interpreted by a cardiologist.
Some common abnormalities seen on an electrocardiogram include:
- Irregular or abnormal heart rhythms (arrhythmias)
- Heart enlargement
- Heart changes that can occur if high blood pressure goes untreated or is inadequately treated
- Patterns consistent with coronary heart blockages or heart attack (myocardial infarction)
There is no special preparation for this test.
Cardiac Catheterization/Angioplasty
A cardiac catheterization, also known as a “cath”or angiogram, is a test that determines if there are blockages in your heart’s arteries (coronary arteries). Heart valve problems, overall heart function, and other congenital heart abnormalities are also evaluated on this test. This test is performed by a specially trained cardiologist assisted by specially trained nursing and technical staff, and includes continuous ECG and blood pressure monitoring.
You may have already had a test showing there is a heart problem. When you have a cardiac cath to evaluate your coronary arteries, the cath will show precisely where blockages are, how severe they are, and how many arteries are involved; this information will be more detailed than information obtained from non-invasive tests. When you have a cardiac cath to evaluate a heart valve, additional information is obtained that is not available on other types of tests, including direct measurement of pressures and gradients in the heart.
Sometimes the cardiac cath proves there is not a significant problem with the heart, even though non-invasive tests suggested there was an abnormality. The results of the cardiac cath will help the cardiologist determine the best treatment for you.
Be aware that if a significant coronary artery blockage is found, it is often possible for the cardiologist to open the blockage during the cardiac cath procedure. An angioplasty may be performed, where a tiny balloon is inflated inside the artery to open the artery at the point of blockage. A stent is often placed at the same time to hold the artery open once the catheter is withdrawn.
Overview of the Procedure
A cardiac cath is generally a safe procedure, but as with any invasive procedure, there is a small amount of risk. Your cardiologist will discuss the risks of the procedure before you sign a consent form.
During the procedure, a long, thin plastic tube called a catheter is passed through the blood vessels of the body to the heart. The entry site for the catheter is the arm or the groin area of the leg. Contrast agents or “dye” can be injected through this catheter into the heart arteries and chambers while x-ray pictures are taken. Angioplasty and stenting can also be performed.
The procedure is relatively painless since there are no nerve endings inside the blood vessels to feel the catheters being moved back and forth. The only significant discomfort is the local anesthetic injected into the skin before the catheters are placed. Patients are given as much sedation as they need to be relaxed during the test.
The entire procedure usually takes under one hour to complete.
Before the Cardiac Cath
You will be asked some questions regarding your health, including any allergies to food, medicine, or x-ray dye. If you are pregnant or think you may be, tell your doctor or nurse. You will need blood tests and an electrocardiogram (ECG) before the test. You will need to sign a consent form indicating that you understand the procedure and any risks that might be involved.
Please bring a list of the names and dosages of your current medications. Alternatively, you may bring your pill bottles with you.
Your doctor or the cardiac cath coordinator will give you special instructions regarding your medications. You may be instructed to stop taking blood thinners such as Coumadin several days prior to the test. Anti-platelet medications, such as aspirin or Ticlid, should not be discontinued unless your doctor specifically instructs you to do so. Dosages of insulin or pills for diabetes may be reduced the morning of the test. You may be instructed to stop taking Glucophage (Metformin) three days before the test. Take your usual medications the morning of the test with water unless otherwise directed. If you have any questions, do not hesitate to ask your doctor.
Do not eat or drink anything after midnight on the day of the angiogram. On the day of the test, please remove any hairpins, earrings, or nail polish. You may wear hearing aids or glasses during the procedure. At the hospital, you may be given medication to help you relax before the procedure. Your nurse will insert an intravenous line, or IV, in your arm that will be used during the procedure.
During the Cardiac Cath
In the catheterization laboratory, you will lie on a table under an x-ray camera. You will see television monitoring screens and a moving x-ray tube or camera. You may be able to see the pictures taken of your heart during the test. Small pads, called electrodes, will be placed on your chest to monitor your heartbeat. The hair at the site where the catheter is inserted will be shaved and the skin cleaned with a special soap. A large drape will then be placed over your body to create a sterile field where the doctor will work. The doctor will then numb the skin in the arm or the leg. Additional medicine may be given in your IV to help you relax. When the skin is numb, a guide wire is passed through a needle inserted into the artery in the leg or arm. A short introducer tube called a sheath is then placed over the guide wire through which the coronary catheters can be passed. There is no pain after the skin is numbed.
When the x-ray pictures have been taken, the catheters are removed. The sheath may be left temporarily in place. It will be removed after you are moved back into your bed. The entire procedure generally takes less than one hour. If an angioplasty is necessary, it can usually be done at the same time as the cardiac catheterization.
Angioplasty is one of the most widely used interventional therapies for opening blockages in the arteries of the heart. During the angioplasty, the cardiologist guides a small balloon to the site where the artery is blocked. Once the balloon is inflated, the plaque material that is clogging the artery is compressed to the side, creating a wider channel for blood to flow. Often a metal stent is placed to reinforce the opened channel and help prevent the artery from closing back down. With any angioplasty, there is a small risk of the artery closing down at the time of the procedure, which can lead to a heart attack. Therefore, an operating room and a cardiac surgeon are always available, should urgent open-heart bypass surgery be necessary. Patients who have an angioplasty done should expect to stay in the hospital overnight, but can usually be discharged home the following morning.
After the Cardiac Cath
Once you are back in bed, the sheath will be removed. After the sheath is pulled, firm pressure is immediately applied to the artery by hand or with a C-clamp device for 20 to 40 minutes. This will allow the puncture site in the artery to seal over with a small blood clot. A sandbag will then be applied over the groin site for 4 to 6 hours to make sure the artery heals properly. Bedrest will also be needed for these 4 to 6 hours after the procedure. In some cases, the artery can be sealed with a mechanical plug. In these cases, the sandbag is not usually necessary and patients need only a few hours of bed rest. After a period of time, you will be asked to get up and walk. If there are no problems, you will be discharged home at that time. Your cardiologist will review the results of the cardiac cath with you and your family, and future treatment plans will be discussed. You should leave the hospital with a complete understanding of the test results and any follow-up instructions. Your primary care physician will be notified of the test results as well.
Going Home
Unless you need other treatment right away, you can go home after the cath. You will need a ride since you cannot drive with the arm or leg used for the cath. Also, some of the medicines used to help you relax may leave you feeling a little lightheaded.
As soon as you arrive home from the hospital, you should remain at rest except to use the bathroom. You can return to your normal routine the following day unless otherwise instructed by your doctor. The bandage may be carefully removed the next day. You may shower or take a bath at that time. Do not plan to do any heavy lifting (greater than 20 pounds) or exercise for two full days after the test. You should not plan to drive for one to two days after the test.
Fatigue is common for a day or two after the procedure. You may have a small lump or bruise at the catheterization site. The area may be sore for a few days. Generally, all these types of symptoms resolve in a few days or weeks. In the unlikely event that you have any bleeding from the catheter site, you should apply manual pressure immediately and have someone contact your cardiologist. If serious problems develop, you should be transported to the nearest hospital by ambulance.
Finally, be sure to call your doctor if you have any of the following problems:
- Numbness or severe pain in your arm or leg
- Bleeding or redness at the catheter site
- Fever greater than 100 degrees
- Hives, or swollen lips or tongue
- Shaking, sweats, or chills
- Shortness of breath or chest pain
- Difficulty voiding or blood in the urine
We hope this information has been helpful, but should you have any further questions or concerns, please feel free to call our office at (203) 265-9831 and ask for the Cath Coordinator.
Dr. Lee provides useful information on cardiac catherization. Click below to watch his video.
Transesophageal Echocardiogram (TEE)
During this test, a small tube-like probe will be passed into your esophagus so that clear ultrasound pictures can be taken of your heart structures. A tiny ultrasound element at the tip of the probe allows images of your heart to be obtained using sound waves. The test is performed by a specially trained cardiologist assisted by a registered cardiac technologist and nursing staff, and is done with continuous ECG and blood pressure monitoring.
In special circumstances, this test is used to obtain more or clearer information than can be obtained on a standard resting echocardiogram. In this case, the TEE probe is in the esophagus and very close to the heart, so images are very clear. A TEE can also be used to guide other procedures, such as cardioversion, or bubble studies to evaluate for abnormal communication between heart chambers.
Assessment for congenital heart defects, heart valve disease, heart muscle disease, artificial heart valve function, and the presence of blood clots in the heart are common reasons for performing a TEE.
Your throat will be numb, and you will be given intravenous sedation so that you will be comfortable throughout the test. The test itself lasts approximately 20 minutes. However, please allow approximately three hours; additional time is necessary in order to prepare you for the test, as well as to observe you for a while when the test is over.
Instructions
- If your doctor requests a special blood test prior to the TEE, be sure to get it done on the specified date. You will be contacted by MidState Medical Center (map) prior to your appointment. If you miss the phone call, the number for Cardiodiagnostics is (203) 694-8215.
- Have nothing to eat or drink from midnight on prior to your TEE appointment.
- If you have diabetes or some other special medication consideration, ask your doctor for special instructions on how to take your medication on the day of the test.
- You will not be able to drive after the test for the remainder of the day, so bring someone with you to transport you home.
- You will need to report to MidState Medical Center’s Cardiodiagnostics on Lewis Avenue in Meriden at the scheduled time.
We hope this has been helpful, but should you have any further questions or concerns, please feel free to call our office at (203) 265-9831 and ask for the TEE coordinator.
Dr. Dinker provides useful information on transesophageal echocardiography. Click below to watch his video.
Electrophysiology Evaluation (EP Study)
An EP Study is an in-depth evaluation of the heart’s electrical system, or how the heart generates and conducts electrical impulses. This type of test is often used to diagnose complex abnormal heart rhythms (arrhythmias) or when treatment for an arrhythmia is unsuccessful.
A doctor who is specially trained in electrophysiology conducts this test in a hospital setting, assisted by specially trained nursing and technical staff, with sophisticated monitoring of the ECG, blood pressure, and blood oxygen. Mild sedation is given; special catheters are inserted into blood vessels in the groin, arm, or neck area, and advanced to the heart using x-ray guidance.
A catheter is used to stimulate the heart in specific areas to see if arrhythmias can be produced. This helps the doctor to understand what is causing the arrhythmia, and to determine the most appropriate treatment.
Sometimes an ablation is performed at the time of the EP Study. In this case, the doctor tries to destroy the tiny area of heart tissue that is producing or sustaining the arrhythmia. This is done by delivering electrical (or cold) energy to the problem area through one of the catheters.
The length of time varies from procedure to procedure, and can sometimes take 4 hours or more to perform. The patient may be kept overnight. If the patient is released on the day of the procedure, he or she must be accompanied by a driver.
A special preparation is required for this test, which is given by the doctor (or his assistant) when the procedure is scheduled.
Speak to your cardiologist about electrophysiology options.
Pacer/ICD Assessment, Resynchronization Therapy
We offer a wide array of services for patients who have abnormal heart rhythms (arrhythmias) or heart conditions requiring a pacemaker or ICD to be placed and maintained. This is a specialty area of cardiology. The information contained on this page pertains only to patients who have been told by a doctor that they require a pacer or ICD. Not all heart conditions will require a pacer or ICD.
Cardiologists and Electrophysiologists are the two kinds of doctors who specialize in the diagnosis and treatment of heart conditions that may require pacers or ICDs. This team works together to diagnose the heart condition, arrange surgical placement of the appropriate device, and provide ongoing monitoring and support for the device.
For certain heart conditions, the diagnosis is made with a simple electrocardiogram (ECG). Other times the diagnosis is more challenging and may require an electrophysiology study, or EP Study, to be performed. You can read a description of both on our website. Once a heart condition is diagnosed, the doctor may recommend a pacer, an ICD, or a device that does both. All of these are called “devices.”
Pacers and ICDs are similar in that they are all tiny devices that are surgically implanted under the skin of the chest. This requires a short-term stay in a hospital setting. The “device” contains a tiny generator housing a battery and a computer chip that can store information about heart function. A lead wire(s) runs from the device to the heart tissue, either under the skin or through a nearby blood vessel. These devices are comfortable, help people return to their normal daily activities, and are easy to monitor and maintain. The specific function of each device is discussed below.
Once a device is implanted, it is checked periodically and non-invasively by placing a small wand on the chest called a programmer. The programmer allows the doctor to test the battery life, read the information stored on the computer chip, and make adjustments to the device settings. Think of it like your TV remote control!
What device do I need?
In a normal heart, the heart’s natural pacemaker generates tiny electrical impulses. These impulses are conducted through the heart via the “conduction system” (special heart cells that can transmit electrical impulses). The electrical impulses cause the heart muscle to contract and pump blood into the body.
Implantable pacemakers or “pacers” are necessary when disease of the heart’s conduction system prevents the heart’s natural pacemaker from doing its job. Sometimes the heart’s natural pacemaker stops generating the appropriate electrical impulses. Other times the heart’s conduction system can no longer transmit the impulses along. Pacers will help in both of these situations; the pacer lead(s) are positioned so that they can generate and deliver tiny electrical impulses to the proper area(s) of the heart in order to maximize the pumping action of the heart muscle.
ICD stands for Implantable Cardioverter Defibrillator. These devices deliver a slightly greater electrical charge to the heart than a pacer and are used to restart the heart or to interrupt certain dangerous sustained arrhythmias.
Not everyone who needs a pacemaker will need an ICD; pacer/ ICD combination devices are available if indicated.
Another application for pacemakers is Cardiac Resynchronization Therapy, or CRT. The CRT device is a special pacer with more than one lead. It is also called a BiV (pronounced bi-vee) pacer, or biventricular pacer. This type of pacer is used to get both ventricles (or “pumping chambers”) of the heart to pump at the same time. When the ventricles work together, it results in more effective forward blood flow to the body, and can improve symptoms associated with advanced heart failure. Not everyone needs this type of pacemaker. CRT/ ICD combination devices are also available.
Preparation
There are special preparation instructions prior to implantation of a device which will be given by the doctor (or doctor’s assistant) at the time the procedure is scheduled.
Follow-up Care
Patients are given a wallet card with information about their devices. It is important to keep this card accessible and in a safe place. Healthcare providers may need this information during examination or treatment.
We offer appointments several times per month for the ongoing monitoring and support of these implantable devices. More frequent monitoring may be recommended if a patient becomes symptomatic, or as a device ages. Depending on the device, sometimes transmissions are also made over the phone. It is very important to attend the recommended appointments. There is no special preparation for these appointments, and patients will be comfortable during these brief checkups.
We hope this has been helpful, but should you have further questions or concerns, please feel free to call us at (203) 265-9831 and tell the operator you need information on our pacer/ ICD services.
Mobile Testing Services
We have several accredited mobile sites where testing is performed.
Mobile testing services include:
- Echocardiograms
- Carotid Duplex Ultrasounds
- Ankle Brachial Index Testing (ABIs)
- Holter and Event Monitors
- Ambulatory Blood Pressure Monitors (ABPMs)
If your practice or facility is interested in setting up on-site testing services, please contact our Testing Lab Supervisor or one of our physicians at (203) 265-9831 for Wallingford testing. For all other offices, call our main scheduling number at (860) 522-0604.
Please bring your insurance card and co-pay (if any) to your appointment.
If you have any questions or concerns about your test, please call:
All Offices: (860) 522-0604
Wallingford: (203) 265-9831