Electrophysiology

Millions of people experience irregular or abnormal heartbeats, called arrhythmias, at some point in their lives. Most of the time, they are harmless and happen in healthy people free of heart disease. However, some abnormal heart rhythms can be serious or even deadly. Having other types of heart disease can also increase the risk of arrhythmias.
While a cardiologist is equipped to deal with most cardiovascular disease, sometimes the input of a cardiovascular subspecialist is required. Electrophysiology is one such subspecialty.
An electrophysiologist is a cardiologist who focuses on testing for and treating problems involving irregular heart rhythms, also known as arrhythmias. They examine your heart’s electrical system, which sends an electrical signal through your cells to regulate heart rate and rhythm.
In August of 2023, we were pleased to welcome electrophysiologist, Dr. William Perucki to our team.
Meet Dr. William Perucki

Dr. Perucki is a Connecticut native who attended the University of Connecticut where he graduated in 2004 with a BA in Business Administration. He worked for six years in the field of finance and accounting and then decided to pursue a lifelong dream of becoming a physician. Proud of his Polish heritage, he chose to attend medical school at Jagiellonian University Medical College in Krakow, Poland. He graduated in 2014 and returned to Connecticut where he completed his Internal Medicine Residency at the University of Connecticut.
Dr. Perucki completed his cardiology fellowship at Hartford Hospital. He went on to complete an additional fellowship in Clinical Cardiac Electrophysiology at Temple University in Philadelphia, Pennsylvania.
The Role of an Electrophysiologist
Dr. Perucki is an expert at diagnosing and treating issues of the heart’s electrical system. Using both non-invasive and minimally invasive techniques, he performs testing of the electrical system of the heart to determine the best treatment, which can be either a medication or procedure. Procedures may include implanting a pacemaker or defibrillator to maintain a natural heart rhythm or performing a catheter-based radiofrequency ablation to eliminate abnormal heart rhythm.
Who Needs to See an Electrophysiologist
Patients are primarily referred to Dr. Perucki by cardiologists or primary care providers who suspect abnormal heart irregularities. He sees patients with heart palpitations, slow heart rhythm, irregular, fast, or erratic heartbeat, or who have passed out for no reason.
Diagnosing Heart Rhythm Abnormalities
One of the initial steps Dr. Perucki takes is to observe. This may involve having the patient wear a monitor at home for 2-4 weeks. Or, for those patients who had a stroke, he may implant a small monitor. This is done right in the office, and it can monitor the heart for 3-4 years to look for abnormal heart rhythms.
Sometimes, Dr. Perucki will suggest medication as the initial approach to see if that can correct the issue. Medication can be effective in approximately 50-60% of the cases. Other times, he may take a wait-and-see approach to determine if the heart abnormalities stabilize over time or require more extensive treatment.
For patients with serious or life-threatening issues, or those that may prefer a more definitive treatment, a procedure may be the optimal approach.
Types of Procedures
For patients diagnosed with a fast heart rhythm, Dr. Perucki may perform a catheter-based radiofrequency ablation to eliminate abnormal heart rhythms. This minimally invasive procedure is done in a hospital setting, using a series of catheters that allow him to identify, target, and eliminate abnormal electrical signals from your heart.
For patients diagnosed with slow rhythms, Dr. Perucki may perform a minor surgical procedure to implant a pacemaker to supplement or “rewire” the heart to get it to work the way it should.
For a patient with a weak heart facing the risk of sudden death, Dr. Perucki may perform another minor surgical procedure to implant a defibrillator which can monitor the heart’s rhythm 24/7 and if necessary restore a normal rhythm.
These procedures are done at Hartford Hospital and Midstate Hospital. They are done on an outpatient basis and most patients go home the same day.
Helping Patients Find the Best Solution
Dr. Perucki considers his role as an advisor. He shares, “My job is to present options to patients once a diagnosis is made. Together, we look at the treatment choices and it is a shared decision-making process. While many of the minimally-invasive procedures can result in dramatic improvement, this is not always the optimal path and I work with patients to consider all the options.”
Learn About Dr. Perucki
Pre and Post Instructions for Insertion of Pacemaker/ICD
Pre procedure for Pacemaker/ICD
1-2 weeks ahead:
- Please have blood work done within 1-2 weeks of your procedure date.
The night before:
- Do not have anything to eat or drink after midnight the day prior to procedure.
- Use the special soap, Hibiclens (chlorhexidine), with scrub brushes the night before and the morning of the procedure on your left/right chest and arm.
- You will receive a phone call the day before procedure (Friday if procedure is on Monday) between 3pm and 6pm with arrival time and location; schedule for the day is not known before then and we are unable to provide a time before this.
The morning of the procedure:
- Medication Management:
- If you use insulin or any oral medications for diabetes, please do not take them the morning of the procedure.
- Talk to your doctor about additional medications you should avoid taking prior to the procedure.
- Take approved medications with a sip of water the morning of the procedure.
- Continue your present medical regimen unchanged up until this day, unless otherwise noted.
After the procedure:
- You will need a ride home with a chaperone after the procedure which will most likely be a same-day discharge.
If you have any questions regarding your procedure, please call our office at:
(203) 265-9831 or (860) 522-0604.
Post procedure for Pacemaker/ICD
Important phone numbers:
- Surgeon/Electrophysiologist’s office: (203) 265-9831 or (860) 522-0604
- They are available Monday–Friday, 8am–4:30pm.
- Our answering service is available after hours for emergencies and can contact the on-call physician for any urgent or emergent matters.
Symptoms:
- If you have recurring symptoms similar to those before your device was implanted (dizziness, near-fainting, fatigue), or you receive a shock from your ICD, please call the office at the number listed above.
Care of Your Incision:
- Monitor your incision daily for:
- Redness
- Swelling
- Drainage
- Opening of the skin at the incision line
- Worsening pain
- Fever higher than 101° F and/ or chills
If you experience any of the above, call your surgeon/ electrophysiologist’s office immediately.
Dressing and Care:
- If dressing is still present, remove the gauze dressing 24 hours after surgery. There may be steri-strips or a special adhesive over the incision. Do not remove these; they should come off gradually with showering. If after 2 weeks there are still strips or glue present, you can gently remove these using baby oil.
- If you have steri-strips, do not get them wet for 3 days after discharge. If you have the special adhesive, you may shower 24 hours after discharge.
- Do not use alcohol, lotions, powders, or ointments on the incision.
Management of Pain:
- It is normal to have some bruising or mild swelling around the incision/ pocket for a few weeks after surgery. If needed, you can take Tylenol (acetaminophen) every 6 hours for discomfort.
- Never take more than 3,000mg of acetaminophen in 24 hours.
- If your discomfort is severe or is not relieved by acetaminophen, please call your surgeon’s office immediately, as this may indicate there is a problem.
Restrictions:
- Do not raise your device arm above shoulder height or reach behind your back for 3 weeks. Do use your device arm normally in other ways to avoid muscle stiffness and pain in the shoulder.
- No sudden, vigorous pulling, pushing, or chopping movement with your device arm for 6 weeks. This includes mowing the lawn, snowplowing, golfing, tennis, bowling, swimming, and all contact sports.
- Do not lift more than 10 pounds (approximately 1 gallon of milk) with your device arm for 6 weeks after surgery. This includes children, grandchildren, and pets!
- You may be asked not to drive for a certain period of time. This is different for everyone. Please ask your doctor when you may resume driving.
- Avoid dental cleaning for 6 months after implant, if possible. Please notify your dentist that you have a device; sometimes antibiotics are prescribed for dental procedures.
- Sexual activity can be resumed when you feel ready.
- You can resume your normal activities. Walking is healthy and recommended. Increase activity as tolerated.
- If you were given an arm sling, only use for 24 hours, then remove. You can wear it at night pinned to your nightshirt if concerned about lifting your arm over your head during sleep.
Call Your Primary Cardiologist if You Experience Any of the Following:
- Weight gain of more than 3 pounds in 24 hours, worsening shortness of breath, or chest pain not related to your surgical site.
Remote Monitor/Transmitter information:
- You should have received a remote monitor at the time of your implant. Please plug in your remote monitor immediately when you return home after your hospital stay. Instructions are available in the remote monitor box.
- If you have difficulty setting up the monitor, or have questions, please call the device company’s toll-free number listed on the box or monitor.
Follow-up:
- You will need a wound check appointment 2 weeks after your procedure. We will check your device then. We will check your device again 3 months after your procedure. Please call our office if there are any concerns.
Pre and Post Instructions for an Ablation
Pre procedure for Ablation
1-2 weeks ahead:
- Please have blood work done within 1-2 weeks of your procedure date.
The night before:
- Do not have anything to eat or drink after midnight the day prior to procedure.
- You will receive a phone call the night before procedure (Friday if procedure is on Monday) between 3pm and 6pm with arrival time and location – schedule for the day is not known before then and we are unable to provide a time before this.
The morning of the procedure:
- Medication Management:
- If you use insulin or any oral medications for diabetes, please do not take them the morning of the procedure.
- Talk to your doctor about any additional medications you should stop prior to the procedure.
- Take approved medications with a sip of water the morning of the procedure.
- Continue your approved medical regimen unchanged up until this day, unless otherwise noted.
After the procedure:
- You will need a ride home with a chaperone after the procedure which will most likely be a same-day discharge.
If you have any questions regarding your procedure, please call our office at:
(203) 265-9831 or (860) 522-0604.
Post procedure for Ablation
Important phone numbers:
- Surgeon/Electrophysiologist’s office: (203) 265-9831 or (860) 522-0604
- We are available Monday–Friday, 8am–4:30pm.
- Our answering service is available after hours for emergencies and can contact the on-call physician for any urgent or emergent matters.
General Information:
- Do not drive for 3 days after the procedure.
- For a few weeks, or even up to 3 months, after your ablation, you may feel occasional skipped beats or a sensation that your arrhythmia is starting up. These symptoms are very common and usually decrease in frequency over time. If you have irregular beats that do not go away or think that your arrhythmia has returned, please call our office.
Activity:
Although the puncture sites heal quickly, there is a small chance of bleeding from the puncture site where the catheters were placed during your procedure.
- For at least 3 days, do not lift, push, or pull anything heavier than 10 pounds, or do any exercise that causes you to hold your breath and bear down with your abdominal muscles.
- One week after the procedure, you may resume your regular activities, including sexual activity. We suggest that you begin your exercise program at half your usual routine for the first few days and gradually work back up to your full routine.
If you are on Coumadin/ warfarin or any other prescribed blood thinners:
- For at least 7 days, do not lift, push, or pull anything heavier than 10 pounds, or do any exercises that causes you to hold your breath and bear down with your abdominal muscles.
- Ten days after your procedure, you may resume your regular activities, including sexual activity. We suggest that you begin your exercise program at half your usual routine for the first few days and gradually work back up to your full routine.
Care of the Puncture Sites:
- Do not take a tub bath, sit in a hot tub, or swim until the puncture site is healed. This usually takes about a week.
- Leave the dressing(s) on the site(s) until the day after the procedure.
- A small bruise or bump (around the size of an almond) may form under the skin at the puncture site. This is common and generally disappears in 3-4 weeks.
- Keep the site clean and dry. You may get the site wet the day after the procedure. Use regular soap and water and pat the area dry; do not rub.
- Do not use alcohol, ointment, lotion, powder, or creams on the puncture sites.
- Monitor the sites daily for signs of infection: fever, redness, swelling, warmth, new soreness, or drainage. Report any of these symptoms to your electrophysiologist.
When to Call Our Office:
- If you experience increased weakness or inability to do regular activities.
- If you experience difficulty breathing or chest pain.
- If symptoms re-occur that were present prior to ablation, such as lightheadedness, palpitations, fluttering, fainting, or near fainting.
- If you have questions about your arrhythmia medications.
If You Had an Atrial Fibrillation Ablation:
- You will be asked to have your warfarin level (INR) drawn more frequently after your ablation. Please see your general discharge instructions for this schedule.
- You may have more frequent follow-up visits with your electrophysiologist. Please see your general discharge instructions for your appointments.
If you have any questions regarding your procedure, please call our office at:
(203) 265-9831 or (860) 522-0604.
Implantable Cardioverter Defibrillator (ICD)
Click here for a decision aid for Implantable Cardioverter-Defibrillators (ICD)
This is for patients with heart failure considering an ICD who are at risk for sudden cardiac death (primary prevention).
Replacement of Implantable Cardioverter Defibrillator (ICD)
Click here for a decision aid for replacement of Implantable Cardioverter-Defibrillators (ICD).
This is for patients that already have an ICD and are considering replacement.
Cardiac Resynchronization Therapy with Defibrillation (CRT-D)
Click here for a decision aid for Cardiac Resynchronization Therapy with Defibrillation (CRT-D)
This is for patients with heart failure who are getting cardiac resynchronization therapy and considering defibrillation.
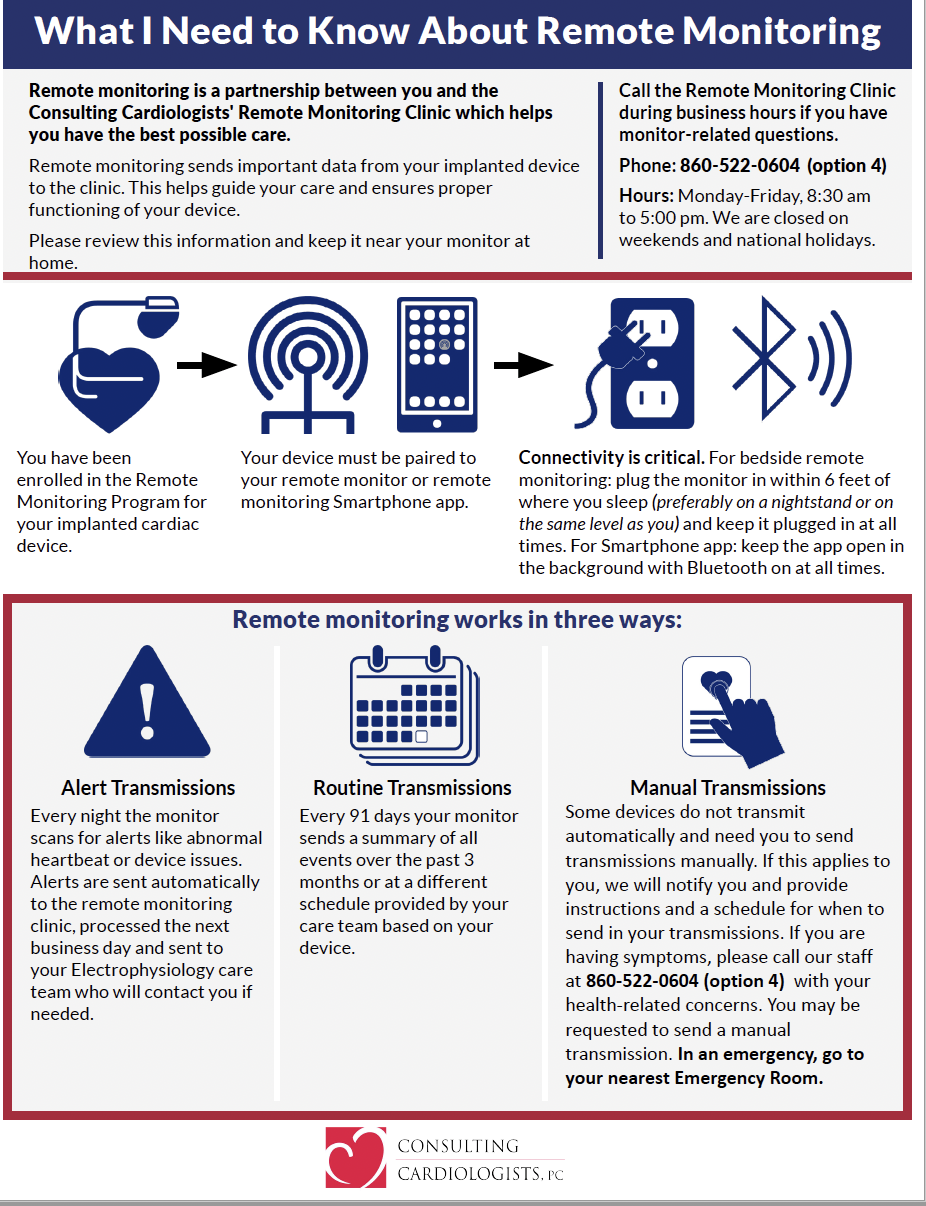
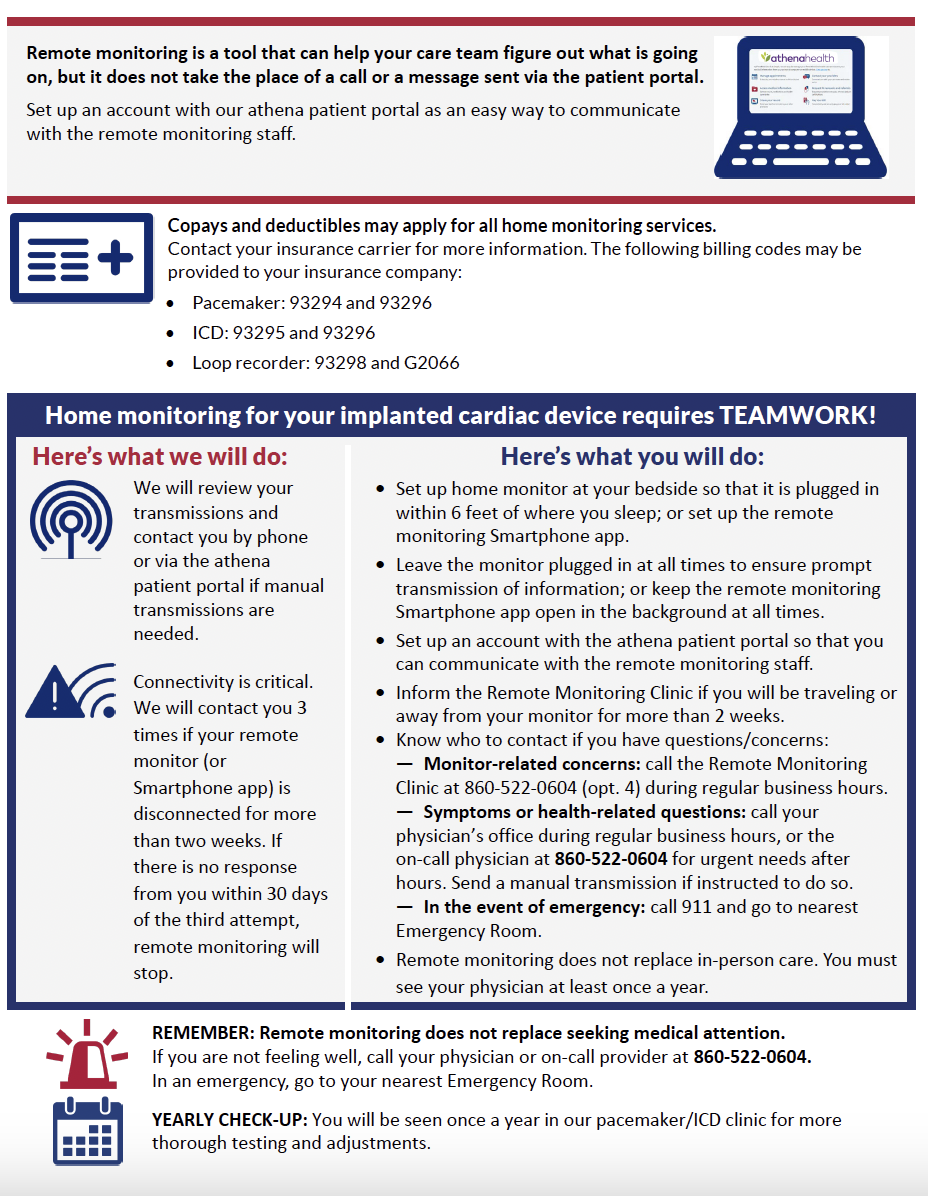
What to Know About Remote Monitoring
Below is some helpful information about monitoring from home.
Education Materials
Videos
Below are a number of patient videos created by electrophysiologist Dr. Joshua Cooper.
What is Atrial Fibrillation (AF)
How do we treat Atrial Fibrillation (AF)
What is Wolff Parkinson White Syndrome and how do we treat it
What are premature ventricular contractions (PVCs) and how do we treat them
